Reporter: Claudia Villalobos / Photos: Courtesy of CBG – 09/06/2025
The Center for Genomic Biotechnology is developing more effective weapons against drug-resistant bacteria
According to researcher Jessica Lizbeth Ortega Balleza, bacteria can quickly develop resistance—even to newly released antibiotics.
The discovery of penicillin and the development of various antibiotics marked a turning point in modern medicine, saving millions of lives worldwide. However, antimicrobial resistance has become an ongoing and escalating public health challenge. The World Health Organization (WHO) estimates that by 2050, antimicrobial resistance could cause up to 10 million deaths annually. The rapid emergence of multidrug-resistant and pan-resistant bacteria has prompted scientists worldwide to seek innovative ways to combat this phenomenon. Resistance typically arises from genetic mutations that allow bacteria to evade the effects of drugs, making infections increasingly difficult to treat. At the Center for Genomic Biotechnology (CBG), researchers from the Pharmaceutical Biotechnology Laboratory have joined the WHO’s global strategy to tackle this crisis. Their work focuses on identifying inhibitors of Type IV secretion system proteins, which play a critical role in spreading antibiotic resistance genes within bacterial communities.
As part of her postdoctoral research at CBG, Dr. Jessica Lizbeth Ortega Balleza—under the guidance of Dr. Gildardo Rivera Sánchez—has been investigating bacterial resistance mechanisms. She explains that bacteria can exhibit two types of resistance: natural (intrinsic) resistance to certain antibiotics, and acquired resistance, which occurs when resistant bacteria transfer genetic material to previously susceptible strains.
Acquired resistance is particularly concerning because it spreads faster than the development of new antibiotics. For this reason, Dr. Ortega Balleza is focusing on the repurposing of existing, FDA-approved drugs to block the mechanisms that allow resistant bacteria to pass resistance genes to susceptible microorganisms. Even last-resort antibiotics are showing diminished effectiveness shortly after reaching the market, as bacteria employ various strategies to mutate and adapt, she noted.
To identify the most promising compounds for inhibiting genetic transmission via conjugative pili, Dr. Ortega Balleza used bioinformatics tools to screen approximately 11,000 pharmaceutical compounds.
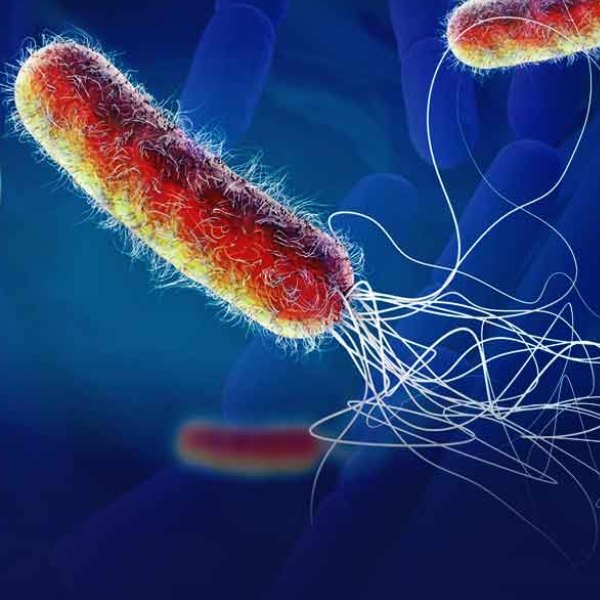
Following a molecular docking analysis, 127 drugs were selected based on their favorable pharmacokinetic and pharmacodynamic profiles. These candidates showed the potential to inhibit the formation of conjugative pili—hair-like appendages on the bacterial surface that facilitate direct contact and genetic exchange between bacteria.
“We found that the target bacterium possesses proteins involved in gene transfer. This allows us to focus on disrupting the formation of the bridge between two microorganisms,” she explained.
To further refine the selection, the candidate for Mexico’s National System of Researchers (SNII) narrowed the list to the top five drug candidates, which will soon undergo in vitro testing.
Dr. Ortega Balleza highlighted the urgency of addressing resistance in six high-priority pathogens—Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp.—collectively known as ESKAPE organisms for their ability to “escape” the effects of antibiotics.
“Some of these bacteria are Gram-positive and have more complex, harder-to-inhibit gene transfer mechanisms than Gram-negative bacteria. For this reason, we are initially focusing on Gram-negative species, which have thinner cell walls and facilitate more efficient gene transfer. Specifically, we are currently studying Escherichia coli and will expand to other species later,” she said.
Plasmids—circular DNA molecules—are key vectors in the spread of antibiotic resistance, as they can horizontally transfer resistance genes through a process called conjugation.
Identifying the presence of proteins involved in this mechanism allows researchers to determine a bacterium’s potential to spread resistance. Molecular biology techniques such as polymerase chain reaction (PCR) help detect these genetic components.
In upcoming in vitro tests, researchers will expose a well-characterized resistant strain—with known resistance genes—to a fully susceptible strain. Both strains will be incubated together, along with the selected drug compound, to evaluate whether it can inhibit the conjugative pilus and thus prevent gene transfer.
Dr. Ortega Balleza explained that the experiment is designed to simulate the transfer of resistance between bacteria. Two controls will be used: sodium azide, to which the resistant bacterium is vulnerable, and an antibiotic that the sensitive strain cannot withstand. If the drug under investigation successfully inhibits conjugation, the sensitive strain will not acquire resistance.
This outcome would provide strong evidence that the compound can disrupt gene transfer between bacteria—an essential step in halting the spread of resistance., lo cual es crucial para combatir la propagación de la resistencia a los antibióticos.
While in silico results have been encouraging, Dr. Ortega Balleza emphasizes that computer simulations alone are not conclusive. She remains optimistic that at least two of the five top-ranked drugs will demonstrate effective inhibition of gene transfer during the experimental phase, which could significantly reduce the spread of acquired resistance. Dr. Rivera Sánchez added that, depending on the in vitro results, researchers may later consider modifying chemical substituents to further enhance the compounds’ ability to block gene transfer.
Currently classified at Level III of Mexico’s SNII, Dr. Rivera Sánchez cautioned that bacteria are constantly evolving to evade therapeutic options. However, blocking the transfer of resistance genes could mark a major advancement in the fight against antibiotic resistance.
The researchers stressed that while pharmaceutical innovation is essential, public awareness and responsible behavior also play a vital role in curbing antimicrobial resistance.
Basic hygiene practices—such as frequent hand washing—can significantly reduce the bacterial load and transmission. They also highlighted the importance of completing antibiotic treatments as prescribed, avoiding self-medication, and steering clear of illegally purchased antibiotics.
Prescription regulations are in place to prevent the misuse of antibiotics, especially in cases of viral infections where antibiotics are ineffective.
Ultimately, combating antibiotic resistance requires coordinated action from the pharmaceutical industry, the scientific community, and the general public to preserve the effectiveness of current treatments for as long as possible.